Glue Vein Treatment
Treating venous reflux with medical grade adhesives.
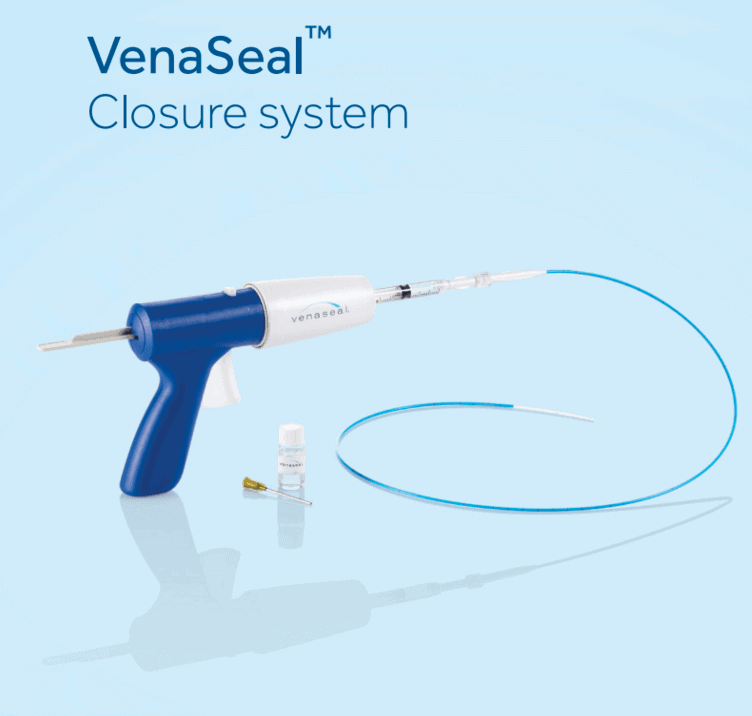
The VenaSeal Closure System is the most modern non-surgical procedure used to safely and effectively treat varicose veins. The Venaseal Procedure by Medtronic is an adhesive based treatment for chronic vein disease in the thighs and lower legs. This minimally invasive surgical procedure is approved by the Food and Drug Administration (FDA) to permanently eliminate varicose veins and venous reflux. Since venous reflux is the direct cause of the physical symptoms associated with long-term vein disease, resolving it successfully is especially important.
The VenaSeal procedure uses surgical adhesive to shut down veins that aren’t working properly. This adhesive is a cyanoacrylate, meaning that it’s in the same class as what is commonly known as “Super Glue.” It permanently bonds to the walls of the vein and can’t travel elsewhere in your circulatory system. It’s completely inert, won’t trigger allergic reactions or an immune response, and it can’t break loose and lodge elsewhere in the body. It’s entirely safe, and in fact, is commonly used in some types of brain surgery.
“There’s essentially no risk . . . We’ve approved this system based on impressive safety data. It’s not our official stance, but if it’s safe enough to be used in brain surgery it’s safe enough to be used anywhere.” . . . “this adhesive approach doesn’t rely on heat so there’s no damage to surrounding tissue. Surgeons in the field are finding that there’s very little recovery time or downtime with this technique. There usually isn’t even bruising.”
Vascular Surgeon Dr. William Maisel, director of the FDA’s Center for Devices and Radiological Health.
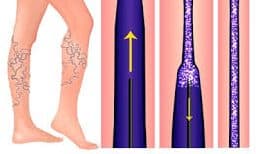
The VenaSeal closure system is used to treat the symptoms of chronic vein disease, which is technically named Chronic Venous Insufficiency (CVI), which is also called Symptomatic Venous Reflux disease. Chronic Venous Insufficiency in the lower extremity superficial venous system is often the underlying cause of painful varicose veins. The VenaSeal procedure uses a cyanoacrylate adhesive (CA) to close the vein. During treatment cyanoacrylate adhesive is introduced directly into the vein being treated. The glue begins to permanently bond with the vein wall where it undergoes a hardening process (sclerosis). Once fully hardened the incompetent vein is sealed shut along its entire length and gradually is reabsorbed by the body. Due to the nature of the venous system the blood is immediately diverted into nearby healthy veins. The final effect is identical to that produced by the RF and EVLT techniques.
Cyanoacrylate adhesive eliminates the need for multiple injections of large amounts of tumescent anesthesia around the vein. Instead, there is typically only one injection of local anesthesia. VenaSeal eliminates CVI by sealing shut veins which aren’t working properly. VenaSeal works best on the larger veins of the thighs and lower leg. In the majority of cases, this will be the Greater Saphenous Vein (GSV) or the Small Saphenous Vein (SSV). Since the saphenous veins connect to practically all other veins in the legs treating one or both can eliminate nearly all the symptoms of CVI.
The VenaSeal™ Closure System also removes the need for thermal energy to permanently close the veins eliminating the risk of thermal injury. This means that the risk of nerve or skin damage is also reduced. Healing time is decreased since the medical adhesive sets within minutes. Patients can return to normal activities more rapidly. Post treatment compression stockings are not required and most patients return to work and normal activity right away. The entire procedure can be performed in just 20-30 minutes without the need for a general anesthetic.
To date the VenaSeal system is arguably the least invasive treatment in use today.
Benefits of the VenaSeal Closure System
- No general anesthetic required
- No medications must be taken to prepare the patient for the procedure
- Immediately alleviates symptoms and improves appearance
- It’s nearly 100% effective
- It’s minimally invasive
- It’s as permanent and safe as other competing techniques
- Most people report only mild discomfort during the procedure
- The procedure can be performed within 20-30 minutes – no need to miss a whole day of work!
- Recovery time is minimal, most people can return to work and resume normal immediately, including exercise.
Two other closure techniques are currently in use today, yet, VenaSeal is by far the least invasive. Only a small amount of local anesthetic is needed at the incision sites. This means very few needle sticks are involved which increases comfort and reduces the risk of infection. Bruising is almost nonexistent.
Before & After VenaSeal Photos

How the VenaSeal System works.
Common symptoms associated with damaged vein valves
Every larger vein in the body has a series of one-way valves which ensure that blood flows in the right direction, towards the heart. When these valves become damaged, weakened, or stretched out this results in backflow. This is the ultimate cause of all Chronic Venous Insufficiency and thus the cause of all the symptoms associated with leg vein disease.
These include but are not limited to:
- Pain and discomfort
- Tired and achy legs
- Excessive swelling
- Varicose veins
- Spider veins
- Skin changes such as discoloration or scaly patches
- Cramping
- Restless Leg Syndrome (RLS)
- Bleeding from surface veins
- Ankle ulcers, which can occur in severe, untreated vein disease
Common symptoms associated with disease of the superficial leg veins include:
- Discomfort, ranging from a minor ache to moderately intense pain
- Heaviness, which increases when standing for long periods
- Swelling
- Cramping
- Restless Leg Syndrome (RLS)
- Changes in skin color
- In advanced cases venous stasis ulcers can form on the insides of the ankles.
The VenaSeal Closure System can entirely eliminate, or greatly relieve, these symptoms by effectively treating venous reflux. This stops the progression of vein disease as well.
Undergoing the Venaseal Procedure

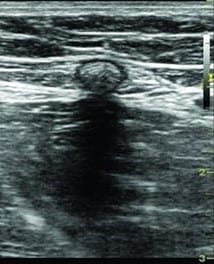
Almost all vein disease is diagnosed by an ultrasound exam. Doppler ultrasound can directly measure venous reflux, making it the ideal tool for the job. Unlike X-Rays there’s no radiation involved so the process is entirely safe. Your surgeon will then review the results of the exam to determine whether or not you’re a good candidate for the VenaSeal procedure.
You won’t need to take any medications to prepare for VenaSeal. Only very small amounts of local anesthetic, usually lidocaine, are needed for pain control. To begin the procedure several tiny incisions are made which allow access to the vein. These incisions are about 1/8 of an inch long, small enough so that stitches aren’t necessary.
Completing the treatment is simple. The surgeon inserts a small catheter to deposit medical grade adhesive at strategic points in the vein, sealing it shut. The blood begins to flow through nearby healthy veins which instantly eliminates venous reflux.
Are There Side Effects Or Complications After a VenaSeal Procedure?
Yes, VenaSeal can have complications and side effects like any other medical procedure. Luckily they are rare and mild, so you don’t have to be really worried. But just for safety purposes, it’s important to know about them, here are some of them:
1. Mild Pain and Discomfort: Patients can experience a little discomfort or pain at the treated site, this resolves in just few days though!
2. Bruising or Swelling: Bruising and swelling are also common, but they won’t last really long either, they should be gone in a week or two.
3. Skin Discoloration: Skin can have temporary skin discoloration or darken at the treatment site but it also fades as you recover.
4. Infection: Risk of an infection with a treatment like this is quite rare, but if it happen it may happen at the injection side if the area isn’t cleaned properly or bacteria manage to reach it somehow. If it happens then make sure to inform your doctor about it, if should be fine with proper care and antibiotics.
5. Deep Vein Thrombosis: This complications is much rarer than infections, so be not afraid. However, in some cases there’s a chance of blood clot forming after a vein treatment. If you notice it’s symptoms, you better inform your doctor. Compared to Vein stripping, the chances of DVT are much less with VenaSeal though.
6. Allergic Reaction: If somehow you are allergic to the medical adhesive then you can experience allergic reactions, so it’s important to inform your doctor about any allergies you have.
Can VenaSeal Treat Both Large and Small Veins?
Yes, VenaSeal is able to treat both large and small varicose veins which makes it a really versatile treatment. However, it’s most effective on larger veins, so if your veins are larger then VenaSeal can be a to-go treatment!
What Happens after the VenaSeal Procedure
After the treatment your surgeon will clean the treated site and apply a bandage on it to prevent excess bleeding. After that, you can go home by yourself. With VensSeal there is a very short recovery time, which means you can return to your daily activities the next day! For a better recovery, your doctor will recommend some low impact exercises like swimming, jogging, walking, and biking. Since all these exercise can help you improve blood circulation in your legs.
How soon can I resume normal activities after the Venaseal procedure?
After the Venaseal procedure, most patients can resume normal activities immediately or within a short period of time. Unlike traditional vein treatments, the Venaseal procedure typically does not require a recovery period or downtime.
Patients are usually encouraged to engage in light activities such as walking immediately after the procedure to promote blood circulation. However, it is important to follow the specific instructions provided by your doctor. While you can resume normal activities, you may be advised to avoid strenuous exercises, heavy lifting, or prolonged standing for a short period of time, usually around 1 to 2 weeks.
Are multiple sessions of the Venaseal procedure required for complete treatment?
In most cases, the Venaseal procedure can be completed in a single session, providing effective treatment for varicose veins. Unlike some other treatment options, the Venaseal procedure does not typically require multiple sessions or follow-up treatments.
During the procedure, a special medical adhesive is used to seal the affected vein, which helps to redirect blood flow to healthier veins. This process is usually completed in a single treatment session, and the treated vein gradually becomes scar tissue over time.
However, it’s important to note that each patient’s condition is unique, and the number of sessions required may vary depending on the extent and severity of the varicose veins. In some cases, additional treatments or complementary procedures may be recommended for optimal results.
Is the Venaseal procedure permanent, or will the treated veins eventually reappear?
The Venaseal procedure is designed to provide long-lasting results, and in many cases, the treated veins do not reappear. The procedure involves using a medical adhesive to seal the affected vein, which causes it to close off and eventually become scar tissue. This effectively redirects blood flow to healthier veins.
Will There Be Discomfort?
If you experience any kind of pain at the treated area you can elevate your legs, this will help you improve blood flow in your veins which will reduce pain. Over the counter medication can also be helpful in relieving discomfort. If the pain or discomfort isn’t well managed on your own, then do not hesitate to contact your doctor.
What Should I Avoid During Recovery?
To ensure optimal results from your VenaSeal procedure:
- Avoid strenuous activity right after the treatment,
- Avoid overdoing normal activities like cycling, walking and swimming,
- Avoid alcohol and tobacco consumption,
- Don’t rest all day, being active, as recommended by your provider, promotes circulation.
Vein Glue FAQ
Two other minimally invasive technologies are currently being used to treat Chronic Venous Insufficiency (CVI). Both are safe, effective, and yield results which are indistinguishable from those of VenaSeal. They are, however, slightly more invasive and cause more downtime. Also note that compression stockings must be worn for approximately 2 weeks following these procedures.
- Endovenous Laser Treatment (EVLT). This procedure uses highly focused laser energy to produce heat which damages the walls of the vein being treated. This permanently seals the vein..
- Endovenous Radiofrequency (RF) Ablation. This procedure is almost identical to EVLT. The only real difference is that Radiofrequency (RF) energy is used to produce the results.
Yes, but there’s a good chance you’ve already met them.
Most insurance companies will ask about conservative treatments, which include:
- Modifying activities. If you experience symptoms severe enough to seek treatment, you’ve most likely had to curtail your physical activities somewhat. This can be as simple as having to take a 90 second rest after standing for long periods.
- Elevating the legs. If you’ve sat in a recliner chair or propped your legs up in any way, you’ve met this requirement.
- Wearing compression stockings. The majority of patients who seek professional treatment have tried compression hose at some point. If you haven’t, simply wear compression stockings for a few months before scheduling your procedure.
- The use of over the counter (OTC) pain relievers such as Motrin (ibuprofen), Aleve (naproxen sodium), and Aspirin.
When benefits are denied you’ll receive a written explanation known as an Explanation of Benefits (EOB). This will state the reason your claim was rejected. A good example is failing to try conservative treatments first, i.e. not wearing compression hose.
The solution is usually simple. Wear prescription stockings for the required period of time, then schedule an appointment for a re-evaluation.
Venaseal is even less invasive than its minimally invasive counterparts, Radiofrequency (RF) Ablation and Endovenous Laser Therapy (EVLT).
While Venaseal is a newer technology, it’s been proven safe, causes very little pain or discomfort, and has very brief recovery times.
Tumescent anesthesia is a local anesthetic that is used in other procedures used to treat varicose veins. It is injected around the vein being treated and requires multiple injection sites. Since the VenaSeal Closure System uses painless “glue” to treat the vein, it does not require the use of tumescent anesthesia. Instead, only one injection of local anesthesia is typically needed.
Most patients report little to no pain during the procedure.
None!
The VenaSeal™ Closure System was designed to make the recovery process as quick and easy as possible. Patients can resume normal non-strenuous activities immediately.
Results are immediate. Within 12 months after the procedure the vein turns into fibrous connective tissue that occludes the vein permanently, as seen on this ultrasound image:
There are several current treatments used in the medical community to treat chronic venous insufficiency.
Conservative treatments attempt to correct or improve the condition without surgery.
They include:
- Compression Stockings,
- Exercise
- Leg Elevation
- Unna Boots
These modalities have the potential to slowly improve minor symptoms and have very few side effects.
Surgical procedures are more aggressive, showing more immediate results.
Surgical stripping is a common procedure where the great saphenous vein (GSV) is split at its confluence with the common femoral vein. The term stripping refers to the removal of a long vein segment. This modality has been in use for over 100 years. It is typically conducted in the operating room and requires general anesthesia. It often requires up to 4 weeks of recovery time. There is a long incision scar that can lead to discomfort and will require wound care. After treatment, you will need to wear a compression stocking.
Thermal therapies apply heat (or other energy forms) to the veins. They can lead to:
Endothermal heat-induced
- hematoma,
- hyperpigmentation,
- nerve injury,
- scarring,
- thrombophlebitis,
- thrombus (EHIT)
These therapies may result in the need to wear compression stockings.
Cyanoacrylate is FDA approved and is widely used as a medical tissue adhesive, but, it also has an antimicrobial effect against gram-positive organisms.
These bacteria include:
- anthrax (Bacillus anthracis),
- diphtheria (Cornynebacterium diphtheriae),
- pneumococci,
- staphylococci (“staph”),
- streptococci (“strep”).
It has been used safely on millions of patients and according to a 1986 study, there is no danger of carcinogenicity in humans.
Cyanoacrylate is used in a variety of medical procedures as a hemostatic agent or to “glue” tissues together in a surgical wound. it is widely used in orthopedic procedures to affix hardware. Additionally it has been used in plastic surgery for blood vessel anastomoses, wound closure, application of skin grafts, or hemostasis.
Surgeons have found that cyanoacrylate has many advantages including:
- binding properties are not affected by moisture or blood,
- easy to use in the operating room,
- eliminates the need for compression stockings,
- encapsulated by the body just like a foreign body,
- ideal viscosity,
- polymerization starts when it comes into contact with blood or plasma,
- quick polymerize,
- retains strong adhesion,
- soft and elastic bond,
- stimulates an inflammation in the vessel wall causing occlusion.
Is it any wonder that professionals who are looking to improve their patients’ experiences are starting to use cyanoacrylate?
Clinical Studies on VenaSeal System Results
The VenaSeal procedure was studied in 2011, 2012 and 2013. The results show VenaSeal to be safe and effective, with consistent results.
- A high rate of closure was found in the studies. Studies were conducted after the procedure at different intervals (from 2 days to 3 years). After six (6) months, the closure rate varied from 92.9% to 98.9%
- VenaSeal has an acceptable safety profile. Documented side effects are minor and infrequent.
- Using the VenaSeal system eliminates the need for post procedure compression stockings.
- Tumescent anesthesia is not required for the VenaSeal system.
- The VenaSeal system does away with the risk of thermal injury.
- Patients who undergo the The VenaSeal procedure are able to return to normal activities quickly.
- VenaSeal is the only non-thermal, non-sclerosant, non-tumescent system approved for the treatment of chronic venous insufficiency in the United States.
Chronic Venous Insufficiency (CVI) or Symptomatic Venous Reflux Disease can lead to painful and irritating symptoms. There are several drawbacks to the traditional treatment methods of stripping and thermal therapies which can be avoided when using the VenaSeal system.
Vascular Study: full-length cyanoacrylate procedures vs. combined cyanoacrylate-sclerotherapy procedures in the treatment of venous reflux.

During the last 5 years there’s been a surge of interest in cyanoacrylate “vein glue” for incompetent leg veins. One of the main advantages of using vein glue is the almost complete lack of downtime. What’s more, patients aren’t required to wear compression stockings post-procedure. From a patient’s standpoint, this alone is often enough to justify a vein glue procedure such as VenaSeal.
Cyanoacrylate Procedure
Overall, the cyanoacrylate procedure has proven itself to be highly effective and extremely safe. In fact, it can credibly be claimed that these procedures carry almost no risks. Yet, while this may be true, the technique does have its limitations and isn’t appropriate in all cases.
It’s possible to employ vein glue in two distinct methods. The first is full-length application. This involves applying cyanoacrylate to the entire length of the treated vein. When used correctly, this method is virtually 100% effective. It does, however, require large amounts of the expensive adhesive. Alternately it’s possible to use a segmental approach. This entails applying vein glue to strategically selected points along the length of the vein. This is still effective in the majority of cases and is much less expensive.
Researchers at the American Society for Venous and Lymphatic Disorders have proposed a third approach. This combines the ease and minimally invasive nature of segmental vein glue procedures with segmental sclerotherapy. As detailed below, this gives results which are comparable with full-length cyanoacrylate application.
VenaSeal Procedure Study Methods:
The study cohort consisted of 24 patients, 17 women and 7 men, who underwent the combined procedure described above. Patients presented with Chronic Venous Insufficiency (CVI) of the Great Saphenous Vein (GSV). Vein diameters ranged from 8-24 mm with a mean of 9.4 mm. A double-access access catheter was used to apply both cyanoacrylate and an air-sclerant foam, in this case, aethoxysklerol. Various branch veins and perforators were treated via application of cyanoacrylate at junctional areas. No manual compression therapy was delivered during the procedure. After the procedure sterile non-compressive dressings were applied at the access site. Additionally, no compression therapy (compression stockings) were used post-operatively.
VenaSeal Procedure Study Results:
The treated vein was immediately occluded in all 24 patients resulting in the elimination of venous reflux. The amount of cyanoacrylate adhesive used per vein was 10.5-33.7 mg with a mean of 16.1 mg. When averaged, this amounts to approximately 2.9 mg / cm. In comparable full-length procedures the amount of cyanoacrylate used was 24.7-67.0 mg with a mean of 39.9 mg. When averaged, this amounts to approximately 6.0 mg / cm. This means that, on average, 3.1 mg / cm less cyanoacrylate was used in the combined approach.
VenaSeal Procedure Conclusions:
While the study suffered from small sample size, it can be seen that the segmental approach achieved complete vein occlusion in all patients. In both the full-length and segmental approach no anesthesia was required beyond that needed at the access site. No compression therapy was required at any point in the procedure. Most notably, 3.1 mg / cm less cyanoacrylate was needed to complete the segmental approach. This represents a greater than 50% reduction when compared to the full-length method.
The American Society for Venous and Lymphatic Disorders recognizes the need for larger cohort studies. It is further recommended that trials of the above combined approach using non-acrylate adhesive be undertaken.
Important Safety Information – Risks, Warnings, Contraindications, Precautions and Complications of VenaSeal™ Closure System
- Use VenaSeal Closure System as a complete system, never use components separately.
- Should only be performed by endovenous trained Physicians
- For use in superficial truncal veins only (GSV)
- Must have Ultrasound Guidance
Contraindications to using VenaSeal
- Sepsis (blood infection)
- Superficial Venous Thrombophlebitis
- Allergy or sensitivity to cyanoacrylates or VenaSeal adhesive
- Pregnancy
What are the signs of complications after the VenaSeal procedure?
After the VenaSeal procedure, it’s important to monitor for signs of complications. While complications are rare, here are some potential signs to watch for:
- Infection:
– Redness, warmth, or swelling at the treatment site
– Fever or chills
– Pus or unusual discharge from the incision site
- Pain or Discomfort:
– Persistent or worsening pain in the treated area
– Pain that does not respond to over-the-counter pain relievers
- Swelling:
– Significant swelling in the leg or around the treated vein
– Swelling that does not improve with elevation or compression
- Bruising:
– Severe or spreading bruising beyond the immediate area of the procedure
- Numbness or Tingling:
– Numbness, tingling, or a “pins and needles” sensation in the leg or foot
- Skin Changes:
– Changes in skin color or texture near the treated area
– Development of ulcers or sores
- Blood Clots:
– Sudden onset of pain, redness, or swelling in the leg
– Pain or swelling that travels up the leg
How effective is the VenaSeal procedure in treating varicose veins?
The VenaSeal procedure is highly effective in treating varicose veins. Clinical studies and patient outcomes have shown the following effectiveness:
- Success Rates:
– VenaSeal has reported closure rates of the treated veins around 94-98% in the short term (within the first few months post-procedure).
– Long-term studies indicate that these high closure rates are sustained, with effectiveness lasting several years post-treatment.
- Symptom Relief:
– Patients typically experience significant relief from symptoms such as pain, swelling, and heaviness in the legs soon after the procedure.
- Minimally Invasive:
– The procedure is minimally invasive, reducing recovery time and associated risks compared to traditional surgical methods.
- Patient Satisfaction:
– High patient satisfaction rates due to the procedure’s efficiency, minimal discomfort, and quick return to normal activities.
Potential Risks and Complications
Below is a list of the potential adverse effects (e.g., complications) associated with the use of the VenaSeal system. The adverse events associated with the device are similar to those with traditional endovenous thermal ablation procedures. In addition, there are several risks unique to the VenaSeal system due to its material and product design as an implant. These potential adverse events include, but are not limited to, the following:
- Allergy to glue – hives, itching, anaphylactic shock
- Arteriovenous fistula (i.e., an abnormal connection between an artery and a vein)
- Bleeding and infection at catheter insertion site
- Blood clots in deep veins, Blood clots to lungs (Pulmonary embolism)
- Bruising, collection of blood outside the vein
- Infection at the access site
- Itching at injection site
- Leg swelling, hyperpigmentation, visible scars
- Local numbness, pain, inflammation of vein and surrounding area
- Neurological deficits including stroke and death
- Non-specific mild inflammation of the cutaneous and subcutaneous tissue
- Pain
- Paresthesia (i.e., a feeling of tingling, pricking, numbness or burning)
- Phlebitis (i.e., inflammation of a vein)
- Rupture or perforation of vein being treated
- Superficial thrombophlebitis
- Ulceration may occur at the site of injection
- Vascular rupture and perforation
- Visible scarring