What is May-Thurner Syndrome?

It may go by many names, but the potential harm caused by this vein disease can be life-threatening. May-Thurner syndrome is also known as Cockett’s Syndrome or Iliac Vein Compression Syndrome. It primarily attacks a pair of vessels that carry blood in and out of the legs.
The condition places pressure on one of the veins, decreasing the blood flow. The resulting slow blood flow makes you more likely to suffer from a deep vein thrombosis (DVT) in your left leg.
A Problem With the Blood Vessel
Blood vessels are the interstate highway systems of your body. They carry blood from the heart to every part of your body and back again. The oxygen carried by the circulatory system keeps each cell in your body alive. If there is a blockage, an opening, or some other reason that blood cannot reach a cell, that cell will die. This is what happens in deadly strokes and heart attacks.
The arteries are responsible for moving blood away from your heart, and the veins return it. In some spots in the body, your arteries and veins will cross paths. This is typically not a situation that causes problems. That is unless you suffer from May-Thurner syndrome.
Swollen Right Iliac Artery
May-Thurner syndrome is characterized by a swollen right iliac artery. The right iliac artery and the left iliac vein cross in your pelvis. The right iliac artery transports the oxygen-rich blood to your right leg and the left iliac vein carries the blood back out of your left leg toward your heart.
In cases of May-Thurner syndrome, the right iliac artery swells up and compresses against the left iliac vein in the pelvis. The exterior pressure placed on the left iliac vein makes it harder for the blood to freely flow out of the legs. It is similar to pinching a straw while trying to drink from it. You can get a small about of the beverage through the reduced opening, but it takes more time and effort.
What will my Doctor do to Properly Diagnose my May-Thurner Syndrome?
In order to properly diagnose May-Thurner syndrome, your doctor will likely want to:
- Inquire into your medical history.
- Ask about your symptoms.
- Give you a complete physical exam. He or she will examine the area and test your general health (blood pressure, etc.)
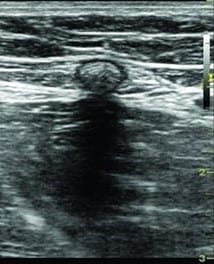
- Employ an imaging test (an ultrasound, echogram, MRI, or venogram) to confirm a suspected diagnosis.
May-Thurner Syndrome Clotting in your Left Leg
The conditions produced by the limited flow of blood are conducive to clotting in your left leg. As the blood is moving more slowly, it will spend more time in contact with the adjacent blood cells and vein walls making it easier to form a bond.
Individuals with this condition are more likely to develop a deep vein thrombosis (DVT) in their left leg. A DVT clot can be quite serious. Not only can these types of clots cause damage by blocking the regular blood flow in your leg, but they can also become life-threatening if they break loose.
When a DVT breaks loose, it will travel through the circulatory system and can find another place to become lodged. If it reaches your lungs, it can cause a life-threatening blockage in the lungs called a pulmonary embolism.
Causes and Risk Factors of May-Thurner Syndrome:
May-Thurner syndrome can affect anyone. There does not appear to be any genetic links associated with May-Thurner syndrome. It is not something that is passed in the genes from generation to generation. Females are more likely to suffer from May-Thurner syndrome because of the stress that pregnancy puts on the pelvis.
Crossing of the blood vessels is natural. Sometimes, however, they are situated in such a way that the right iliac artery pushes the left iliac vein back into the spine. The additional pressure causes the vein to collapse leaving a narrower opening. It is similar to what happens when you step on a garden hose. If the contact with the spine is abrupt, it can injure the vein, causing scarring. The scars will make the interior of the vein even narrower.
You are at a higher risk to get May-Thurner syndrome if you:
- are a woman
- are dehydrated
- have been diagnosed with another medical condition that causes your blood to clot easily
- recently had a baby
- have given birth to more than one child
- use oral birth control
- suffer from scoliosis
May-Thurner Syndrome: Symptoms

Unfortunately, there are very few warning signs for May-Thurner Syndrome. Many people do not realize that they have the condition unless they develop a deep vein thrombosis. Some people report a general pain or slight swelling in the leg, but typically, there are no warning signs.
There are recognizable symptoms for a deep vein thrombosis.
Pay special attention if you notice any of the following:
- The skin on your left leg may appear red or purple
- Your leg feels heavy or tender
- Throbbing in the leg
- Swelling in the leg
- Skin becomes warm to the touch
- Tight pain similar to a cramp or charley horse
- Veins swell in size
If a DVT breaks loose and becomes lodged in your lungs, this is a medical emergency.
Pain in the chest that is made worse when inhaling
Passing out
Coughing up blood
Becoming short of breath or have other breathing problems
A racing heartbeat
All of these are signs of a serious life-threatening condition. Call 911 if you notice any of them.
May-Thurner Syndrome Diagnosis
Your doctor will want to start by asking questions about your condition. He or she will want to know what symptoms you are noticing, under what conditions are they worse or better, and when you first noticed them. After he or she has an understanding of your situation, then the doctor will likely follow up with a full physical exam. He or she will touch different areas of your leg and pelvis identifying if you have common symptoms of a DVT. After that, he or she may order some imaging or lab tests. Your healthcare provider may ask for a blood test, an echocardiogram, or other tests on the circulatory system. Imaging tests may include X-rays, a sonogram, or an MRI.
Is may-thurner syndrome dangerous?
May-Thurner syndrome, also known as iliac vein compression syndrome, is a condition where the left iliac vein in the pelvis is compressed by the overlying right iliac artery. This compression can lead to reduced blood flow and potential clot formation in the affected vein. While it is considered a relatively rare condition, it can be potentially dangerous if left untreated.
If blood clots form in the compressed vein, they can travel to the lungs and cause a pulmonary embolism, which is a serious and potentially life-threatening condition. Symptoms of May-Thurner syndrome may include leg pain, swelling, deep vein thrombosis (DVT), and in severe cases, ulcers or skin discoloration.
Early diagnosis and treatment are crucial to prevent complications. A healthcare professional, typically a vascular specialist, can evaluate the symptoms, perform diagnostic tests such as ultrasound or venography, and recommend appropriate treatment options. Treatment may involve anticoagulant medication to dissolve existing blood clots, angioplasty to widen the compressed vein, or stent placement to keep the vein open and restore normal blood flow.
How long this problem lasts?
The duration of May-Thurner syndrome can vary depending on several factors, including the severity of the compression and the effectiveness of treatment.
If left untreated, the symptoms of May-Thurner syndrome, such as leg pain, swelling, and deep vein thrombosis (DVT), can persist or worsen over time. Additionally, the risk of developing complications, such as pulmonary embolism (a blood clot in the lungs), can increase.
With appropriate treatment, the symptoms and risks associated with May-Thurner syndrome can be managed and reduced. Anticoagulant medication is typically prescribed to dissolve existing blood clots and prevent the formation of new ones. This treatment is usually continued for a period of time determined by the healthcare professional based on the individual’s condition and response to treatment.
Possible Complications of May-Thurner Syndrome:
The primary complication of May-Thurner syndrome is deep vein thrombosis (DVT). By itself, DVT is not a grave concern. However, if a DVT clot breaks loose from the leg, it can move with the blood flow to the lungs. Once in the lungs it could lodge in a pulmonary artery, causing a life-threatening condition known as a pulmonary embolism.
Symptoms of a pulmonary embolism can differ greatly. The severity of the symptoms will vary based on many factors. Some of those are:
- the size of the area of the lung that is involved,
- the size of the clots themselves, and
- whether or not you have any underlying lung or heart disease.
Some of the most common signs and symptoms include:
- Quick onset of shortness of breath that always gets worse with physical exertion.
- Serious “heart attack like” chest pain that may become worse when you take deep breaths, cough, eat, stoop or bend over. Your pain will always get worse when you exert yourself but will not go away when you rest.
- A deep cough that may include blood.
May-Thurner Syndrome Treatment
Due to the serious nature of a deep vein thrombosis clot, if it is discovered that you suffer from May-Thurner Syndrome you should start treatment immediately.
Treatment will target two objectives.
- To treat any current clots.
- To keep new ones from developing.
Your healthcare provider may discuss several different options with you. Those options are discussed below.
Angioplasty and/or a stent:
Many doctors favor using one or both of these methods to help normalize blood flow in patients suffering from May-Thurner syndrome. For angioplasty, you will be given medication to relax you and a local anesthesia will be administered at the entry site (most likely in your groin.) A catheter is guided through a blood vessel to the area of the blockage. Once there, a balloon at the tip of the catheter is inflated. The balloon will push the plaque and stretch the artery open to boost blood flow to the heart. At this point, a stent may be added. A stent is a tiny cylinder made of metal mesh. It holds the vein open so that blood can flow more normally.
Anticoagulants and other Blood thinners:

Drugs that reduce the blood’s ability to clot are frequently used to treat DVT. By “thinning” the blood, they lower the possibility of creating new clots and stop the growth of any clots you already have. There are many types of blood thinners on the market. Talk to your doctor about which one might be right for you. Blood thinners can have serious side-effects.
Iliac Bypass Surgery:
Your doctor can use a vein from your arm to create a detour along which the blood will flow.
IVC Filter:
A vena cava filter is a small device that is inserted in a large vein in your abdomen (called the inferior vena cava). Your doctor might opt for this approach if you cannot take a blood thinner due to another medical condition or if they are ineffective for you. The filter will prevent blood clots from moving through your blood into your lungs. While the filter will not prevent the formation of clots, it will stop them so they do not end up in your lungs and cause a life-threatening pulmonary embolism.
Support Hose:

If you have mild to moderate symptoms and your medical provider does not feel that you are in need of more treatment, he or she might suggest wearing support hose (also called compression stockings.) These tight stockings cover your legs from your knees to your toes and put constant pressure on your lower legs. The constant pressure will ease swelling and improve blood flow.
Surgical Thrombectomy:
This is a type of surgery that removes the blood clot from inside an artery or vein. It is generally reserved for clots that are very large in size or those that are causing severe damage to the tissue. The surgeon will make an incision into the blood vessel. The clot is then removed and the blood vessel is repaired.
Surgery to Reposition the Right Iliac Artery.

During this operation, the surgeon adjusts the position of the artery. He or she positions it so it sits behind the left iliac vein, no longer pressing on it.
Thrombolytic Therapy:
Thrombolytic therapy (also called clot busters) is used by doctors to treat more serious clots. Your medical provider will use a catheter (a thin hollow tube) to apply medication directly to the site of the clot. These powerful drugs can break down a clot in anywhere from a few hours to a few days.
Tissue Sling Surgery:
During this procedure, the surgeon will place some extra tissue between the two blood vessels to act as a cushion between them.
Concerned that you may have May-Thurner Syndrome (also called Cockett’s Syndrome and Iliac Vein Compression Syndrome)?
How does smoking impact the severity or progression of May-Thurner Syndrome?
There are several ways in which smoking will make the May-Thurner syndrome worse and will cause further progression:
- Vascular Damage
Endothelial Dysfunction: Smoking damages the endothelium, the inner lining of blood vessels, leading to dysfunction. This can exacerbate the compression of the iliac vein in MTS, worsening blood flow obstruction.
Atherosclerosis: Smoking accelerates the development of atherosclerosis, a condition where arteries become narrowed and hardened due to plaque buildup. This can further restrict blood flow and increase the risk of clot formation in patients with MTS.
2. Increased Blood Clot Risk
Hypercoagulability: Smoking increases the tendency of blood to clot. In MTS, where blood flow is already compromised due to vein compression, this heightened clotting risk can lead to the development of deep vein thrombosis (DVT), a serious complication of MTS.
Inflammation: Smoking induces chronic inflammation, which can contribute to clot formation and exacerbate venous insufficiency.
3. Impaired Healing and Recovery
Reduced Oxygen Supply: Smoking decreases the oxygen-carrying capacity of blood, impairing tissue oxygenation. This can slow down the healing process and increase the risk of complications post-treatment or surgery for MTS.
Impaired Collagen Production: Nicotine impairs collagen production, essential for wound healing. This can affect recovery from ulcers or surgical interventions related to MTS.
4. Increased Venous Pressure
Venous Hypertension: Smoking contributes to increased venous pressure, exacerbating the symptoms of MTS. Higher venous pressure can lead to swelling, pain, and the development of venous ulcers.
5. Compromised Overall Health
Cardiovascular Strain: Smoking places additional strain on the cardiovascular system, which can compound the effects of MTS.
Managing MTS as a Smoker
Seek Support: Utilize resources like smoking cessation programs, counseling, and medications to help quit smoking.
Regular Monitoring: Regular check-ups with your healthcare provider can help monitor the progression of MTS and manage any complications promptly.
