Leg Ulcer Symptoms
Venous ulcers are both painful and unsightly. Furthermore, untreated ulcers (or ulcers that aren’t treated correctly) almost always lead to more severe medical issues. This condition is a direct consequence of a long history of untreated vein disease of the thighs and lower legs. This underlying disease is known as Chronic Venous Insufficiency (CVI), also known as venous reflux.
These ulcers are almost always located on the inner ankle just behind the “large bump,” aka the medial malleolus. Most ulcers of this type occur adjacent to visible varicose or spider veins. Other vein-related skin changes such as discoloration and thickening of the skin are also commonly seen alongside ulcers.
Venous ulcers present as shallow, inflamed, reddish sores. When infected, which is a distinct risk for all non-healing wounds, they can take on a yellowish color. As mentioned, the worst thing about venous stasis ulcers is the fact that they heal slowly or not at all.
In many cases, venous ulcers have an adverse psychological impact. Non-healing wounds of all types can be extremely painful. They also commonly limit patient mobility and decrease quality of sleep. These are all well-documented risk factors for and potential causes of depression and anxiety.
What causes venous stasis ulcers?
As mentioned above the underlying cause of stasis ulcers is a vein disease called Chronic Venous Insufficiency (CVI). Among clinicians it’s more commonly referred to as venous reflux or simply “reflux.” Put simply, reflux is the backflow of blood in the large veins of the legs.
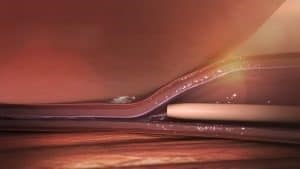
All veins have a series of valves which are designed to prevent blood from flowing down the legs. Over time, leg veins tend to stretch out until the flaps of these one-way valves no longer touch. This causes blood to reverse its course and travel away from the heart, eventually pooling in the legs.
CVI causes a host of problems, ankle ulcers being one of the most severe. More common symptoms include a heavy feeling in the legs, tiredness, and mild-moderate discomfort.
Diagnosing lower leg and ankle ulcers

In nearly all cases no specialized testing is needed to diagnose an ulcer (or venous reflux, for that matter. Instead, the physician uses signs and symptoms to reach his or her conclusion. This is known as a clinical diagnosis.
Yet with this being said medical imaging, particularly Doppler Ultrasound, is useful in determining the severity of a patient’s CVI. This versatile imaging technique can also be used to rule out potentially dangerous blood clots. Using ultrasound, a Registered Vascular Technologist (RVT) can also determine precisely which sections of a vein are affected.
Are there age limitations for treating leg ulcers?
There are typically no strict age limitations for treating leg ulcers. The approach to treating leg ulcers depends more on the individual’s overall health and the specific circumstances surrounding the ulcer. While older adults may experience leg ulcers due to factors like reduced mobility or venous insufficiency, effective treatments can be tailored to accommodate their unique needs. In fact, elderly patients may benefit significantly from appropriate wound care and management. Ultimately, the decision to treat leg ulcers is based on a thorough evaluation by healthcare professionals who consider the patient’s overall health, medical history, and the underlying causes of the ulcer.
What role does compression therapy play in treating leg ulcers?
Compression therapy plays a crucial role in treating leg ulcers, especially those caused by venous insufficiency or chronic venous disease. Here’s how it works:
- Improves Circulation:
Compression garments, such as compression stockings or bandages, apply gentle pressure to the legs. This pressure helps improve blood flow and circulation by assisting the weakened or damaged veins in returning blood to the heart.
- Reduces Swelling:
Compression therapy can reduce edema (swelling) in the affected leg, which is common in individuals with venous ulcers.
- Aids Wound Healing:
By improving circulation and reducing swelling, compression therapy promotes the healing process of the ulcerated area. It helps to supply oxygen and nutrients to the tissues, facilitating tissue repair.
- Prevents Ulcer Recurrence:
Even after an ulcer heals, compression therapy may be recommended to prevent the recurrence of ulcers, as it helps maintain vein function and reduce the risk of future damage.
How long does it take for a leg ulcer to heal with treatment?
The time it takes for a leg ulcer to heal with treatment varies widely depending on factors like the ulcer’s cause, size, and the effectiveness of the chosen treatment. Healing can range from a few weeks to several months.
Costs
Also note that the majority of insurance companies require an ultrasound study before approving the procedure. This is part of establishing “medical necessity,” without which medical insurance companies won’t cover the procedure. Most vein procedures for symptomaric varicose veins are covered.
Treating visible varicose veins.
While this might sound ominous it’s precisely what’s needed. Once these defective veins are removed blood is instantly rerouted to nearby healthy veins which improves overall circulation. This minor, minimally invasive procedure is called a microphlebectomy and actually improves a patient’s overall circulation.
As with most venous procedures a microphlebectomy is performed on an outpatient basis. This typically means either your doctor’s office or an outpatient surgery center. The procedure itself takes about an hour and requires only a local anesthetic such as lidocaine is needed.
Are there specific risk factors that increase the likelihood of developing an ulcer?
Yes, several risk factors can increase the likelihood of developing an ulcer. These factors can contribute to the erosion of the protective lining of the stomach, small intestine, or other parts of the gastrointestinal tract, leading to the formation of an ulcer. Some of the common risk factors include:
- Helicobacter pylori infection:
This bacterium is a significant risk factor for developing peptic ulcers, particularly in the stomach and duodenum.
- Regular use of nonsteroidal anti-inflammatory drugs (NSAIDs):
NSAIDs like aspirin, ibuprofen, and naproxen can irritate the stomach lining and increase the risk of ulcers.
- Smoking:
Cigarette smoking is associated with a higher risk of developing peptic ulcers.
- Alcohol consumption:
Heavy alcohol consumption can irritate the stomach lining and increase the risk of ulcers.
- Family history:
Having a family history of ulcers or a genetic predisposition to developing ulcers may increase an individual’s risk.
- Age:
The risk of developing ulcers tends to increase with age, especially in people over 60.
- Stress:
While stress itself may not directly cause ulcers, it can exacerbate symptoms in individuals already prone to ulcers.
Can ulcers be linked to other gastrointestinal conditions or diseases?
Yes, ulcers can be linked to other gastrointestinal conditions or diseases. Some of the common gastrointestinal conditions that may be associated with the development of ulcers include:
- Helicobacter pylori (H. pylori) infection: This bacterium is a significant cause of peptic ulcers, which can affect the stomach or the first part of the small intestine (duodenum).
- Gastroesophageal reflux disease (GERD): Chronic acid reflux can lead to irritation and damage to the esophagus, potentially causing ulcers in the esophageal lining.
- Inflammatory Bowel Disease (IBD): Conditions such as Crohn’s disease and ulcerative colitis can cause inflammation and ulceration in various parts of the gastrointestinal tract.
Vein Treatment
To begin, ultrasound images are used to evaluate the vein in question (and establish medical necessity for insurance purposes). The area is numbed with lidocaine and the surgeon then makes tiny vertical incisions to access the diseased vein. At this point the vein is removed using specialized surgical tools. It’s important to note that a microphlebectomy is very minimally invasive. The access incisions are only millimeters long and usually don’t require stitches. Scarring is minimal to nonexistent.

After the procedure the area is wrapped tightly in sterile dressing. In the days following the procedure wearing compression stocking is necessary. it’s necessary for a patient to wear compression stocking in the days following the procedure. This reduces discomfort, swelling, bruising, and aids in healing. Recovery is very rapid, and most patients are able to return to work the same day if necessary. After about 2 weeks the patient can resume all activities, including strenuous exercise.
Can ulcers be related to gastrointestinal bleeding?
Yes, ulcers can be related to gastrointestinal bleeding. Peptic ulcers, which include gastric ulcers in the stomach and duodenal ulcers in the upper part of the small intestine, can cause bleeding when they erode blood vessels. Gastrointestinal bleeding from ulcers may lead to symptoms such as dark, tarry stools (melena), vomiting blood (hematemesis), or blood in the stool.
How does smoking impact the development and healing of ulcers?
Smoking can negatively impact both the development and healing of ulcers. Here are some ways in which smoking affects ulcers:
1. Increased Risk: Smoking is a recognized risk factor for the development of peptic ulcers. It can contribute to the weakening of the protective lining of the stomach and duodenum.
2. Delayed Healing: Smoking can slow down the healing process of existing ulcers. The chemicals in tobacco can impair blood flow to the gastrointestinal tract, hindering the body’s natural ability to repair damaged tissues.
3. Complications: Smoking is associated with a higher risk of complications related to ulcers, such as gastrointestinal bleeding. The combination of smoking and ulcerogenic factors can lead to more severe outcomes.
4. Reduced Effectiveness of Treatment: Smokers may respond less effectively to ulcer treatments compared to non-smokers. Quitting smoking is often recommended as part of the overall management plan for individuals with ulcers.
Can certain medications increase the risk of ulcers?
Yes, certain medications can increase the risk of ulcers. Nonsteroidal anti-inflammatory drugs (NSAIDs) are a notable example. These medications, including aspirin, ibuprofen, and naproxen, can irritate the stomach lining and potentially lead to the development of ulcers.
Other medications that may increase the risk of ulcers include certain oral corticosteroids and anticoagulants (blood thinners). Additionally, some medications used to treat osteoporosis, known as bisphosphonates, may pose a risk of irritation to the esophagus.

