Three Steps to Healthy Legs
If you suffer from tired, swollen, heavy, aching legs or itchiness, cramps, restless leg syndrome, lumps or bleeding during shaving, you may have varicose veins. We offer multiple treatment options for problematic veins around the calves, thighs, eyes, hands, nose, abdomen and pelvic areas.

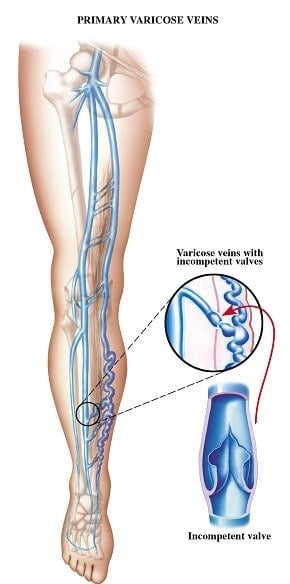
Varicose veins affect up to 30% of the American adult population, mostly in women but they can affect men as well. Age, heredity, pregnancy, occupation (standing or sitting) and genetics can increase the chances of varicose veins. Blood circulates to the legs through arteries and returns to the heart through veins. When you run or walk, the muscles surrounding the leg veins act as a pump to push the blood back toward the heart. The valves within the veins stops the blood from going backwards. If these valves are malfunctioning, they leak blood and increase pressure, like a backed up dam, the veins will weaken and bulge, causing them to become varicose veins.
Without proper treatment varicose veins can cause serious health problems:
- Bleeding – Varicose veins can bleed after minor injury. Pressure, shaving close to the vein, a sandal strap rubbing on the vein or even a hard bump on the leg can cause bleeding.
- Venous Stasis Dermatitis – Lower leg hemosiderin deposits can stain the skin brownish red.
- Phlebitis – A very painful inflammation of the veins of the lower leg. This often leads to cellulitis and ulceration and breakdown of the skin.
- Venous Ulcers – Over time the hemosiderin deposits create poor quality unhealthy skin. This discolored skin eventually breaks open and the resulting wound is called an ulcer.
Our 3 Step Guide to Healthy Legs
STEP 1 – ASSEMBLE INFORMATION

Larger varicose veins are usually easier to spot. However, determining where the vein originates from and the extent of the damage is more challenging. To do this, we conduct tests at our ACR (American College of Radiology) centers using a color duplex ultrasound scan, which checks for abnormalities and blood flow within the vein. We also use a Doppler ultrasound to create a map of the veins using sound waves, which shows blood flow and determines if the vein is refluxing.
STEP 2 – EXPLAIN OPTIONS
We will discuss all options and create a personalized treatment plan for you. For some patients simply wearing compression stockings will fix the issue, while others may need a more involved treatment, such as:
- Sclerotherapy: These are micro injections that close the vein. The sclerotherapy liquid or foam is a safe, effective and popular treatment for veins around the hands, legs and face.
- External Laser Therapy: This is a cosmetic treatment for spider veins. This laser removes broken capillaries on the legs, thighs, chest, hands and face.
- Radiofrequency Ablation (endovenous laser treatment): This effective treatment uses energy to heat the vein, causing it to close. This is a quick, safe, in-house treatment that provides minimal downtime and irritation. We encourage patients to resume normal activities immediately to increase blood flow. RF Ablation relieves inflammation, swelling and other symptoms and prevents discoloration and bulging veins.

STEP 3 – TREATMENT
At the Advanced Vein Center, our varicose veins specialists use the most innovative technology to comfortably and safely treat veins. Treatments for varicose veins are performed by board-certified doctors and physicians specializing in vein health. Most vein procedures are covered by insurance.
Vein treatment is available near by, call today!
724-987-3220
Treating Chronic Venous Insufficiency (CVI)
Chronic Venous Insufficiency, commonly referred to as CVI, is also called Chronic Venous Disease (CVD). Both terms refer to longstanding vein disease which causes nearly all conditions which affect the veins of the legs. These problems include varicose veins and spider veins. CVI is also responsible for the physical symptoms of achiness, swelling, heaviness, fatigue, cramping, and itching. Problems which aren’t normally associated with vein disease can also be caused by CVI. Notable examples include Restless Leg Syndrome (RLS) and chronic, non-healing leg ulcers.
Treating CVI
When conservative treatments fail, several minimally invasive procedures are currently being used to treat CVI. After taking a thorough history and reviewing your ultrasound exam your surgeon will make appropriate recommendations.
- The smallest varicose veins can be dealt with using a technique known as sclerotherapy. This involves the injection of medications directly into the diseased vein. Known as sclerosing agents or sclerants. these medications cause the veins to collapse. In the following weeks and months they are completely reabsorbed by the body.
- Radiofrequency (RF) ablation is probably the most widely used surgical vein disease treatment available today. Ablation means “to shut down or collapse,” which is exactly what RF ablation accomplishes. An ultra-thin wire catheter is inserted into the vein in question. It is then heated, causing the vein to collapse in on itself. Much as with sclerotherapy, the vein is then absorbed back into the body.
- Endovenous Laser Treatment (EVLT) is very similar to RF ablation. It accomplishes the same goals as RF treatment, the only notable difference being the heat source used. In RF ablation Radiofrequency energy is used to deliver heat. In EVLT, laser energy is used to generate the heat necessary for the procedure.
- An ambulatory phlebectomy, also known as a micro phlebectomy, is the surgical removal of large surface varicose veins. The procedure is straightforward: under local anesthesia, small access incisions are made over the diseased veins. They are then removed using specialized surgical instruments.
- High ligation and vein stripping is an invasive older combined procedure. This procedure has largely been replaced by less invasive procedures. During this procedure, large access incisions are used to tie off diseased veins and physically pull them from the body. General anesthesia is necessary, and recovery times are considerable.
What role does hydration play in leg health?
Hydration plays a crucial role in leg health for several reasons:
- Muscle Function: Proper hydration is essential for maintaining optimal muscle function, including those in the legs. Dehydration can lead to muscle cramps and stiffness, affecting mobility and comfort.
- Circulation: Hydration helps maintain adequate blood volume and promotes proper circulation, which is crucial for delivering oxygen and nutrients to the muscles in the legs. Poor circulation can lead to leg swelling, discomfort, and other issues.
- Joint Health: Hydration helps keep the joints in the legs lubricated, reducing friction and minimizing the risk of joint pain or stiffness.
- Skin Health: Adequate hydration is important for maintaining skin elasticity and preventing dryness or cracking, which can be a concern for the skin on the legs, especially in dry or cold climates.
What are the risks of prolonged sitting or standing for leg health?
Prolonged sitting or standing can pose risks to leg health due to the effects of gravity and reduced movement on circulation and muscle activity. Here are some risks associated with both:
- Sitting:
– Poor Circulation: Sitting for long periods can lead to reduced blood flow in the legs, increasing the risk of blood clots (deep vein thrombosis).
– Muscle Stiffness: Lack of movement can cause muscles in the legs to become stiff and achy.
– Poor Posture: Sitting for extended periods can lead to poor posture, which can contribute to back and leg pain.
– Increased Risk of Chronic Diseases: Prolonged sitting has been linked to an increased risk of obesity, heart disease, and diabetes.
- Standing:
– Varicose Veins: Standing for long periods can increase pressure in the veins of the legs, leading to varicose veins.
– Muscle Fatigue: Standing for extended periods can cause muscles in the legs to become fatigued and achy.
Venous insufficiency prevention
Your likelihood of getting venous insufficiency can be decreased by doing the following actions:
• Regular exercise
• Stop using tobacco.
• A extended period of time spent sitting or standing still is not recommended.
• Keep an eye on your weight
