Eliquis Xarelto Coumadin Warfarin Lovenox
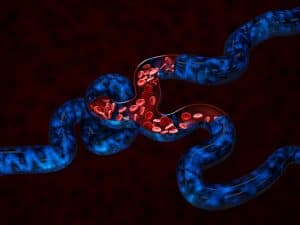
Blood Thinners: What are They?
Blood thinners – Eliquis Xarelto Coumadin Warfarin …- are a useful medicine that physicians use on patients suffering from a variety of conditions. A blood thinner, doesn’t exactly do what it says it does; it’s doesn’t really make your blood thinner but it does facilitate smooth blood flow through the circulatory system. This common medications can also aid in the treatment of blood clots; preventing them from forming or growing in size. Some common uses for blood thinners are:
- treating several types of dangerous heart disease,
- managing heart defects,
- relieving the symptoms of deep vein thrombosis (DVT),
- preventing dangerous blood clots and
- counteracting the clotting properties other medications (for example: oral contraceptives and hormone therapy drugs.)
Protects patients from heart attack or stroke
This FDA approved drug can be used to protect patients at elevated risk of a deadly heart attack or stroke. You should always be aware of the risks of any medicine that you are considering taking. The risk associated with blood thinners is that they can cause you to bleed more than usual if you cut yourself. Doctors prescribe these lifesaving drugs to two to three million Americans each year. The benefits of these common drugs typically trump the possible risks. Nonetheless, in order to manage the potential dangers, you must be aware of them before you start taking blood thinners.
A Tale of Two Blood Thinners
Different types of blood thinners work in different ways. They use different biological functions to achieve the same goal; blood that is less likely to clot and clog the circulatory system.
The first class is called anticoagulants. They are most often available in pill form. Anticoagulants – Eliquis Xarelto Coumadin Warfarin- prevent the blood from coagulating (turning into a solid or semisolid state.) Solid clumps of cells can stick together or to the walls of veins or arteries forming a blockage. Some popular anticoagulants are:
- Eliquis (Apixaban)
- Fragmin, Lovenox, and Innohep (Heparin)
- Pradaxa (Dabigatran)
- Xarelto (Rivaroxaban)
- Savaysa (Edoxaban)
- Coumadin and Jantoven (Warfarin)
- Arixtra (Fondaparinux)
Injection of Blood thinners

The second category of blood thinners are antiplatelets. This class of blood thinner targets the platelets. Platelets are tiny, colorless cells in the blood that are central in the clotting process. When a blood vessel is damaged, a signal is sent out to the platelets. The repairing platelets then respond by converging on the damaged site, plugging and repairing the damage. Most antiplatelets are given in pill form. They include:
- Aspirin
- Effient (Prasugrel)
- Persantine (Dipyridamole)
- Plavix (Clopidogrel)
How do Eliquis Xarelto Coumadin Warfarin blood thinners work?
Blood thinners, despite their name, don’t actually make your blood thinner but they do make it less likely that they will form new clots. While they don’t break up already existing clots on their own, they will keep blood from congealing into new clots. Additionally, they can reduce the pace of growth of existing clots.
The biological pathway of some anticoagulants is to competing with vitamin K production in the liver. Your blood needs vitamin K in order to produce what are called clotting factors. Clotting factors are small proteins that bind the blood cells and platelets together. They are like the glue that turns individual small blood cells into a large mass of cells.
Antiplatelets work a little differently. They stop the colorless platelets from binding onto each other and also keep them from adhering to the walls of your blood vessels. The class of drugs known as antiplatelets are not as strong as the anticoagulants. They are more typically used with patients who are at risk for potential future blood clots, a not to treat existing clots.
When are Eliquis Xarelto Coumadin Warfarin prescribed?
Healthcare providers prescribe blood thinners to about 2 million to 3 million people in the United States every year. They are commonly given to people who have suffered from a heart attack or a stroke. Lowering your blood’s ability to clot, can help reduce the risk that you will have a second heart attack or a stroke.
Individuals diagnosed with a heart or blood vessel disease may also be prescribed blood thinner from their physician. These life-saving medicines can also help those that have an irregular heart rhythm or lupus. Deep vein thrombosis (or DVT) is a life threatening class of blood clot. They most often form in the legs if you are immobile for an extended period of time (for example being confined to bed after an accident or surgery, or on long flights.) You are at a greater risk of developing blood clots if you have an artificial heart valve, are overweight or have recently had surgery. Prescribing blood thinners for those with an atrial fibrillation (AFib or AF) can keep the patient from suffering from a stroke. Stroke prevention is one the most frequent reasons that doctors prescribe blood thinners.
Eliquis Xarelto Coumadin Warfarin for life?
In many situations, patients only need to use blood thinners for a few weeks or months. However, depending on the condition, its severity, whether it is acute or chronic, if you have had recurrences, and the unlying quality of your health you may need to take them as a preventative measure for longer.
Becoming Familiar with the Risks
If you think about it, clotting is one the true wonders of biology. The blood’s ability to transform from a liquid to a semi-solid state in order to stop or reduce bleeding (both internal and external) and bruising is a marvel. How different would life be if our blood didn’t clot? Even small cuts would bleed uncontrollably and require medical attention. Minor head trauma would lead to unstoppable brain bleeding and require surgical attention.
So clotting isn’t a bad thing in every situation. When you get a cut, clotting is what plugs your wound, stopping the blood loss and allowing the blood vessel to repair itself. Blood thinners inhibit the blood’s ability to clot and can lead to some life threatening situations. But don’t worry, when patients are equipped with knowledge, know the warning signs and know how to take precautions, emergency scenarios can be avoided.
If taking blood thinners, you should be extremely cautious when participating in activities that could cause you to injury yourself. Avoid rock climbing, skiing, skating, boxing, football, basketball, and other similar activities. Call your doctor or go to the emergency room right away if you take a fall or hit your head on something. Even if you have not torn your skin, you could be bleeding internally.
How do I know if my blood thinner is working?
You can know if your blood thinner is working through various indicators. Here are some ways to determine if your blood thinner is effective:
- Monitoring tests: Regular blood tests, such as the international normalized ratio (INR) for warfarin or anti-Xa levels for heparin and direct oral anticoagulants (DOACs), can help determine if your blood thinner is within the therapeutic range.
- Symptoms: Improvement in symptoms related to the condition being treated, such as reduced risk of blood clots, stroke, or heart attack, can indicate that the blood thinner is working.
- Prevention of complications: If you are taking a blood thinner to prevent complications, such as stroke in atrial fibrillation, the absence of such complications can indicate that the medication is effective.
Can I safely stop taking blood thinners?
You should not stop taking blood thinners without consulting your healthcare provider, as this can increase your risk of blood clots, stroke, or other serious complications. Your healthcare provider will determine when and if it is safe for you to stop taking blood thinners based on your individual medical history and the reason you were prescribed the medication.
Can I undergo surgery or dental procedures while taking blood thinners?
Yes, you can undergo surgery or dental procedures while taking blood thinners, but it’s important to inform your healthcare provider and dentist about your medication. They will work with you to determine the best course of action to manage your blood thinner therapy during the procedure.
How long do I need to take blood thinners?
The duration of blood thinner therapy depends on the reason for which it was prescribed. Some individuals may need to take blood thinners for a short period, such as after surgery or a clot, while others may need to take them long-term to prevent stroke, heart attack, or other clot-related conditions.
Excessive Bleeding
Call your healthcare provider right away if you are demonstrating any of the following signs of excessive bleeding:
- Having menstrual periods that are heavier than usual
- Discovering blood in your urine or stool
- Episodes of gum or nose bleeds
- Coughing or vomiting up blood
- Feeling of dizziness
- Unusual weaknesses
- Suffering from a severe stomach or headache
Individuals taking an anticoagulant (like warfarin or others) will need to take regular blood tests. These tests will help your doctor adjust your medication if needed. Ask him or her about additional precautions you can take to protect yourself when taking this class of medication. Avoid activities that put you at risk of inflicting head injuries. When you are taking a blood thinner, any type of injury is exceedingly hazardous.
If, while taking warfarin, you do suffer from a injury that leads to a serious bleeding condition, there are some antidotes that can minimize the blood loss and lower the risk of catastrophic blood loss. Healthcare professionals can use vitamin K injections to counteract the effect of anticoagulants. A combination of prothrombin complex concentrate (PCC) and fresh frozen plasma can also be given intravenously. The FDA has also approved the use of Praxbind (idarucizumab) in life threatening emergencies to counteract the anti-clotting effects of Pradaxa.
OTC blood thinners
Other over the counter and prescription medicines and supplements are known to interfere with blood thinners. Make sure to tell all of your doctors (this includes your dentist) about all of the medicines that you take. Do not start taking any new medications without first discussing it with your healthcare provider.
Some foods contain vitamins and minerals that interfere with blood thinners. Because of this, your diet is also very important. Foods that contain high levels of vitamin K (like green, leafy vegetables) should be avoided as they may counteract the blood thinners. Discuss your diet with your healthcare provider.