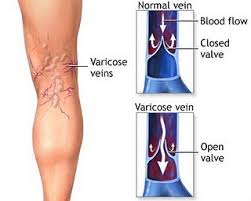
Leaky Valves
“In most cases there’s no single cause, but rather a combination of factors,” says Dr.G “We know that there’s a strong genetic component to having weak, leaky valves. That’s why varicose veins and other vein problems run in families.”
Hormones also play a large role, especially among females. This is the reason why such a large percentage of patient with vein problems are women. The incidence of varicose veins increases with puberty, pregnancy, and menopause. Hormone based birth control, i.e. the pill, also contributes. Of all the above, pregnant women are very prone to vein disease.
Symptoms Of Varicose Veins
Varicose veins may not be painful. Varicose veins can be identified by the following symptoms:
Veins of a dark purple or blue colour
On the legs, veins that seem twisted and bulging, frequently resembling cords
When varicose veins cause pain, the following signs and symptoms may appear:
- Legs that are achy or heavy to the touch
- Lower leg burning, throbbing, muscle cramps, and swelling
- Pain that gets worse after a lengthy period of sitting or standing
- Itching in or around one or more veins
- Varicose veins cause changes in skin pigmentation.
- Varicose veins are comparable to spider veins, except spider veins are smaller. Spider veins are red or blue and are found closer to the skin’s surface.
What Happens If You Ignore Leaky Veins?
Varicose vein complications can include the following, however they are uncommon:
Ulcers. Near varicose veins, particularly near the ankles, painful ulcers can occur on the skin. Before an ulcer occurs, a discoloured patch on the skin generally appears. If you suspect you’ve acquired a leg ulcer, see your doctor right away.
Clots in the blood. Veins deep within the legs can occasionally expand, causing leg pain and edema. If you have prolonged leg pain or swelling, see a doctor since it could be an indication of a blood clot.
Bleeding. Veins close to the skin can sometimes burst. Although minimal bleeding is frequently the result, it necessitates medical treatment.
Risk Factors
Experts are baffled as to why the walls of veins expand and why valves malfunction. This happens a lot of the time for no apparent reason.
Some potential risk factors, however, include:
- Getting over 50 years
- Going through menopause
- Being pregnant
- Having a family history of varicose veins
- Being obese
The risk factors have been linked to an increased incidence of varicose veins:
Females are more likely than guys to suffer from varicose veins. Female hormones may cause veins to relax. If that’s the case, birth control pills or hormone therapy could help.
Am I a good candidate for a venous reflux exam?
If you have in the past been clinically diagnosed with venous reflux or venous valvular insufficiency then you are a good candidate for venous reflux exams. Additionally, individuals who are experiencing symptoms associated with the conditions such as;
- chronic swelling,
- feelings of heaviness or pain in the legs,
- skin discoloration,
- varicose veins or
- venous ulcers.
In many ways pregnancy is the perfect setup for vein conditions. Three main factors are at play.
The first is a matter of blood volume. Since the body is supporting a developing fetus, much more blood is circulating during pregnancy. With more blood comes more pressure. The second is a matter of weight distribution. The fetus and fluid put lots of pressure on top of the pelvis. This works against the flow of blood back to the heart. The third factor is hormonal. During pregnancy women secrete a hormone which makes the vein walls more permeable. As fluid leaves the veins it can add to the amount of swelling already present.
Other main contributing factors are obesity and standing for long periods of time. In general, anything which puts more pressure on the leg veins can damage their valves. This translates directly into vein disease.
How To Prevent Leaky Veins?
Omit salt
The body may retain water if it is exposed to salt or sodium. Leg swelling and leg vein pressure brought on by too much fluid in the legs might weaken vein walls and result in chronic venous insufficiency. Therefore, it is best to avoid them until you are not feeling well.
Skin Moisturizer
A daily moisturizer application can improve the health of your legs while healing dry or cracked skin, even while it doesn’t treat chronic venous insufficiency.
Avoid wearing tight clothing and heels
The risk of developing chronic venous insufficiency is increased by wearing constrictive garments or shoes in the legs. Shoes with high heels can also restrict blood flow to the legs. Your NYU Langone physician might advise donning low-heeled footwear as a result.
Venous insufficiency types
Depending on how severe the symptoms are, chronic venous insufficiency can be divided into three groups.
Stage 1.
This stage is characterized by swelling and alterations in skin pigmentation.
Stage 2.
This stage is characterized by swelling, skin pigmentation changes, and dermatitis.
Stage 3
This stage is characterized by swelling, varicose veins, ulceration, and changes in skin color.
Chronic venous hypertension, which is defined by elevated blood pressure in the veins of the legs, can be brought on by venous insufficiency. Another factor that might cause this illness is blood clots or other vein blockages.
Chronic venous hypertension can result in aberrant capillaries inside the tissues of the legs, leading to ulceration, edema, and hyperpigmentation if ignored. Patches of skin that are affected by this illness darken more than usual.
The best way to avoid venous insufficiency
You can take precautions to lower your risk of having venous insufficiency if your family has a history of the condition:
Never remain seated or upright for extended periods of time. Move about a lot and regularly.
Avoid smoking, and if you do, stop.
Exercise frequently.
Keep your weight within a healthy range.
Are there different types of leaky veins, and if so, what distinguishes them?
Yes, there are different types of leaky veins, each with its own characteristics and causes. Two common types of leaky veins are varicose veins and venous insufficiency:
- Varicose Veins: Varicose veins are swollen, enlarged veins that often appear twisted or bulging. They typically occur in the legs and are caused by damaged or weakened valves within the veins. When these valves fail to function properly, blood can pool in the veins, causing them to become enlarged and leaky. Varicose veins can be painful and may lead to symptoms such as aching, swelling, and skin changes.
- Venous Insufficiency: Venous insufficiency is a broader condition where the veins, often in the legs, struggle to return blood to the heart effectively. This can result from valve damage, blood clots, or other factors. Venous insufficiency can lead to various symptoms, including swelling, skin discoloration, ulcers, and, in severe cases, leaky veins.
Can leaky veins be a sign of a more serious vascular condition?
Yes, leaky veins can sometimes be a sign of a more serious vascular condition or underlying health issue. While leaky veins themselves can cause discomfort and cosmetic concerns, they can also be indicative of broader vascular problems. Some potential connections include:
- Venous Insufficiency: As mentioned earlier, leaky veins can be a symptom of venous insufficiency, which is a more comprehensive condition where veins struggle to return blood to the heart effectively. This can lead to a range of symptoms beyond just leaky veins, including swelling, skin changes, and leg ulcers.
- Deep Vein Thrombosis (DVT): DVT is a condition where a blood clot forms in a deep vein, typically in the leg. It can cause swelling, pain, and warmth in the affected area and may contribute to vein damage and leakage.
Can You Prevent Leaky Valves?
Unfortunately no, it isn’t possible to completely prevent leaky heart valves, but there are some steps you can take if you want to reduce the risk of their development, which can include:
1. Managing Risk Factors:
If you control risk factors like high blood pressure, high cholesterol, and diabetes well then then you can prevent the damage to heart valves over time!
2. Healthy Lifestyle:
You can try daily exercises, maintaining a healthy weight, eating healthy diet rich in fruits, vegetables and even whole grains that support your overall health that makes you much more healthy.
3. Avoiding Infections:
Heart lining can develop an infection called Endocarditis, which can lead to damage of heart valves. But if you manage to have a good dental hygiene and treat infections promptly then you can highly reduce the risks and prevent leaky valves.
What Are The Risk Factors For Developing A Leaky Heart Valves?
Some Risk factors can increase the Risk of developing a leaky heart valve, are here are some of them:
1. Age: As people continue to age, heart valves will naturally become less flexible, weak or damaged which increases the Risk of valve leakage, unfortunately there’s nothing you can do about it.
2. Heart Conditions: Conditions like coronary artery diseases, heart attacks or even infections are really dangerous and can damage the heart valves which leads to leakage.
3. High Blood Pressure: Continuous high blood pressure puts extra strain on the heart and it’s valves, which can lead to dysfunction.
4. Infections: As mentioned earlier, Endocarditis is an infection of the inner lining of the heart which can lead to damage and leakage in the valves.
5. Obesity: Extra weight increases strain and pressure on the heart, which can contribute to valve damage and weakening!