Vein Clinic
Vein disease symptoms, Beaver Pa
Can venous insufficiency be cured? Yes, in our Cranberry Vein Clinic!
- In-office treatment for superficial varicose veins
- Minimally invasive treatment
- Little to no scarring
- Performed under local anesthesia
- No stitches
- No downtime
Venous insufficiency Can be treated simply in a half hour office procedure. Gone are the days of hospital surgeries and prolonged recovery.
How do you know if you have varicose veins?
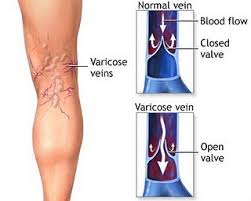
What is a vein disease? When the valves in the veins can’t hold the blood from backflowing and swelling in the legs and ankles, that indicates venous disease.
What disease affects the veins?
- Genetic predisposition
- Lymphedema.
- Atherosclerosis and Peripheral Artery Disease.
- Peripheral Venous Disease and Varicose Veins.
- Aneurysm.
- Blood Clotting Disorders.
- Raynaud’s Phenomenon (Raynaud’s Disease or Raynaud’s Syndrome)
- Buerger’s Disease.
- Blood Clots in Veins (VTE)
- Standing job
- Prolonged sitting
How do you keep your veins healthy? Ways to keep your veins healthy according to venous insufficiency mayo clinic include walking, compression stockings, less sitting and standing, healthy eating habits.
Is venous insufficiency serious?
Venous insufficiency can be serious if left untreated. It becomes progressively worse. Long term varicose veins can even cause leg and ankle ulceration, lymphedema and pain.
chronic venous insufficiency treatment guidelines recommend starting with a doppler ultrasound to assess the severity of the venous disease.
The diet for venous insufficiency includes no alcohol or caffeine.
venous reflux disease pictures can be seen on our website
Chronic venous insufficiency stages
Chronic venous insufficiency:
Symptoms include varicose veins, swelling, or skin color changes on the affected leg. If the condition progresses, leg ulcers can form.
People may experience:
Painful areas: Feet, ankles, lower leg, labia veins
Skin: red or brown darkening of the skin, discolored and thick skin on legs, red or blue swollen or broken blood vessels under the skin, or thick ropey varicose veins
Also common: edema or swelling in extremities, phlebitis, ulcers and cellulitis if left untreated
Personal Changes
You can improve the blood flow in the veins in your legs. Just follow the steps given below and wait for results:
Compression hose
To encourage blood flow, these elastic socks apply pressure to your legs. They are available in various lengths, styles, and tightnesses. Whichever may benefit you the most can be suggested by your doctor.
Movement
Don’t sit or stand still for too long. Stretching or wriggling your legs, foot, and ankles frequently while seated will enhance your blood flow. Take breaks to sit and raise your feet if you stand a lot. Your leg vein pressure will decrease as a result.
Exercise
Exercise also stimulates the blood pump. Walking is a fantastic, easy approach to strengthen your legs and increase blood flow.
The right time to make an appointment with a vein specialist
- At the end of the day or after prolonged standing, your legs begin to feel weak.
Even though it might seem common for your legs to feel weak after prolonged standing, it really isn’t. This weakness can be a symptom of a vein problem. By standing on your legs for prolonged periods of time, varicose veins can make your legs seem heavy and flimsy.
Your legs can be elevated to help you feel less heavy and feeble. However, if you are already in agony, then something is definitely wrong.
- Your daily life is difficult because of your leg pain.
It’s not necessarily indicative of vein problems just because you feel leg pain. Leg pain, particularly painful and throbbing pain, is a result of varicose veins. Additionally, the pain gets worse the more you go about your everyday business while suffering from varicose veins.
You need to make an appointment with a physician to find out if your leg pain is due to damaged veins.
Self-care for vein issues
Your legs’ veins gently send blood back to your heart. Blood tends to collect in your legs because of gravity, especially when you stand up. You might consequently have the following conditions:
- Legs swelling
- Varicose veins
- Changes in your skin, including a skin ulcer (sore), in your lower legs
Schedule Your Exercises
Engage in mild exercise to increase muscle mass and circulation up your legs. Here are a few ideas:
Lay down on your back. Move your legs as though you were biking. Bend the opposite leg while raising one leg straight up. Then alternate your legs.
On the tips of your toes, walk onto a step. Keep your heels hanging over the step’s edge. Lift your heels off the ground while standing on your toes, then let them to touch the step. Make your calf longer. Do this stretch 20 to 40 times.
Go for a little stroll. A 30-minute stroll The ideal frequency is five times a week, however anything might be beneficial.
Go for a calm swim. Take a 30-minute swim: every 5 to 15 minutes.
Avoid remaining still for extended periods of time
To keep the blood in your legs circulating back to your heart when you sit or stand, bend and straighten your legs every few minutes.
Maintain Your Skin
Your skin will remain healthy if you keep it hydrated. Before using any creams, lotions, or antibiotic ointments, see your doctor. Do not use because of potential adverse effects:
- Antibiotics applied topically, like neomycin
- Drying creams like calamine
- A natural moisturizer called lanolin
- Benzocaine or other skin-numbing creams
Keep an eye out for skin sores on your leg, especially near your ankle. To avoid infection, treat wounds straight away.
When to Contact a Physician
Dial your supplier if
- Painful varicose veins
- The severity of varicose veins is rising
- It won’t help if you raise your legs or sit down for a while
Is vein disease more common in certain populations?
Yes, vein disease can be more common in certain populations. Factors such as age, gender, family history, obesity, pregnancy, prolonged standing or sitting, and a sedentary lifestyle can increase the risk of developing vein diseases. Additionally, occupations that involve long periods of standing or sitting, such as nursing or truck driving, can also contribute to the prevalence of vein diseases in those populations. Moreover, individuals with a history of blood clots or who have had previous vein surgeries may be at higher risk. Overall, while vein diseases can affect people of all demographics, certain groups may have a higher predisposition to developing them.
How does aging affect vein health?
Aging can affect vein health in several ways:
- Weakening of vein walls: As we age, the walls of our veins can weaken, leading to decreased elasticity and integrity. This weakening can contribute to the development of conditions like varicose veins and spider veins.
- Reduced muscle strength: Aging often results in a decline in muscle strength and tone. Strong muscles help support healthy blood flow in the veins, so reduced muscle strength can impair circulation and increase the risk of vein-related issues.
- Valve dysfunction: With age, the valves within our veins that help prevent blood from flowing backward can become less efficient or fail altogether. This can lead to blood pooling in the veins, causing varicose veins or venous insufficiency.
- Decreased mobility: Older adults may be less physically active, leading to decreased muscle pump activity in the legs. This reduced muscle movement can impede blood circulation and contribute to the development of vein diseases.
- Thinning of the skin: Aging can cause the skin to become thinner and more fragile. Thin skin is more prone to damage and may be more susceptible to conditions like venous ulcers, which can occur as a result of poor circulation in the legs.
Can vein disease cause infections?
Vein disease itself does not typically cause infections. However, certain complications of vein disease, such as venous ulcers or skin changes, can increase the risk of developing infections.
Venous ulcers are open sores that can develop on the skin, usually around the ankles. These ulcers can be painful and are often slow to heal. The breakdown of the skin associated with venous ulcers can create an entry point for bacteria, increasing the risk of infection.
Additionally, skin changes associated with vein disease, such as dry, itchy skin or thickened skin, can also increase the risk of developing infections. It’s important to promptly treat any skin changes or ulcers associated with vein disease to reduce the risk of complications, including infections.
Are vein diseases life threatening?
Vein diseases are typically not considered life-threatening. However, they can lead to complications that may affect your quality of life and, in some cases, can become serious if left untreated.
One of the most common complications of vein disease is chronic venous insufficiency (CVI), which can cause symptoms such as leg swelling, pain, and skin changes. In severe cases, CVI can lead to venous ulcers, which are open sores that can be painful and difficult to heal.
While vein diseases themselves are not usually life-threatening, the complications they can cause, such as venous ulcers or deep vein thrombosis (DVT), can be serious. DVT is a blood clot that forms in a deep vein, typically in the leg. If a DVT breaks loose and travels to the lungs, it can cause a life-threatening condition known as pulmonary embolism (PE).
How common is vein disease?
Vein disease, including chronic venous insufficiency (CVI) and varicose veins, is common, affecting up to 40% of the population. It is more prevalent in women, older adults, and those with a family history. Risk factors include obesity, pregnancy, prolonged standing, and a sedentary lifestyle. Treatment can improve symptoms and prevent complications.
Vein Clinic FREE Vein Screenings
Call 724-987-3220
REQUEST A FREE VEIN SCREENING
FREE Vein Screenings are available at ALL locations. Vein clinic in Cranberry, Butler vein clinic, and our vein clinic in Beaver.