

Introducing Varithena! A nearly painless way to treat varicose veins and vein disease.
A non-surgical treatment for varicose veins
Varithena, approved by the FDA in 2013, is an clinically proven treatment for varicose veins that combines guided ultrasound with an injectable microfoam is now available for patients at Advanced Vein Center. Currently, it is the only therapy of its kind to have received FDA approval. Varithena effectively improves the appearance of varicose veins caused by vein disease and diseased superficial veins as well as symptoms such as heaviness, achiness, swelling, throbbing and itching (HASTI™ symptoms)1.
When Varithena (1% polidocanol injectable foam) is introduced into a diseased vein via guided ultrasound, the blood within is displaced and the vein begins to collapse. This collapse of the vein stops the backflow of blood from occurring and redirects blood upward and into nearby healthy veins that can handle the optimal flow. After the office treatment, patients can return home and resume most activities the same day. The over 300,000+ Varithena treatments, 12 clinical studies and 25+ peer-reviewed publications demonstrate Varithena’s proven safety and effectiveness2.
For more information, contact us or call/text 724-987-3220.
Can Varithena be used for cosmetic purposes, or is it primarily a medical intervention?
Varithena is primarily designed and approved for medical intervention to treat symptomatic varicose veins. It is not specifically intended for cosmetic purposes. The primary goal of Varithena is to address the underlying medical condition of varicose veins by closing off or sealing abnormal veins, thereby improving symptoms such as pain, swelling, and discomfort.
Varicose veins are often associated with venous reflux, where blood flows backward and pools in the veins, causing them to enlarge and become visibly bulging. Varithena, as a foam sclerosant, works by collapsing and closing these problematic veins.
How long does it take to see results after undergoing Varithena treatment?
The time it takes to see results after undergoing Varithena treatment can vary from person to person. However, some individuals may begin to notice improvements relatively soon after the procedure.
Immediate Effects:
Some individuals may experience immediate relief from symptoms such as pain and discomfort as Varithena works to close off the treated varicose veins. The foaming agent in Varithena helps collapse and seal these veins, addressing the underlying venous insufficiency.
Gradual Improvement:
While some immediate effects may be noticeable, the full results of Varithena treatment often develop gradually over time. The treated veins may take weeks to months to fully close and be absorbed by the body. During this period, patients may observe a reduction in the appearance of varicose veins and an improvement in symptoms.
Follow-Up Assessments:
Healthcare providers typically schedule follow-up assessments to monitor progress and adjust the treatment plan as needed. These follow-up appointments allow the healthcare team to evaluate the effectiveness of the Varithena treatment and address any concerns or additional needs.
Patient-Specific Factors:
The timeline for seeing results can be influenced by various factors, including the extent of the varicose veins, the individual’s overall health, and how well they follow post-treatment care instructions.
Can I Drive Myself Home After A Varithena Procedure?
Generally it’s not recommend to drive yourself home immediately after a Varithena procedure. Despite being a minimally invasive treatment, it’s still not safe to drive on your own, that’s why often doctors will recommend to have someone else drive them home, especially if a sedative or local anesthesia was used during the treatment. But if you still think you can drive, here are some reasons why:
Mild Discomfort: Soreness, rightness, or mild discomfort after the treatment is common. Treated area may make you feel uncomfortable which can make it hard for you to drive.
Compression Stockings: After the procedure, the doctor will probably ask you to wear compression stockings, it can affect the mobility and can make driving much harder.
What Kind Of Veins Can Varithena Treat? Are There Limitations?
Varithena is usually used to treat varicose veins, especially those caused by problems like chronic venous insufficiency, here’s what it can treat and what it can’t:
Veins That Can Be Treated With Varithena:
- Large Varicose Veins: Varithena is an amazing choice for people suffering from large and bulging varicose veins in legs.
- Tortuous Veins: These twisted veins are much harder to treat with other treatment because of their abnormal appearance, but the foam easily flows into the vein which helps the treatment.
- Superficial Veins: These are surface-level veins, they are visible and symptomatic.
Limitations Of Varithena:
- Deep Veins: Unfortunately, Varithena is targeted for only surface level veins, deep vein conditions like deep vein thrombosis is much harder to treat.
- Spider Veins: Varithena’s main targets are larger veins, which is why it’s typically not used for smaller spider veins. Which is why other treatments like Sclerotherapy are considered much better options for it.
- Severe Vein Disease: In case of serious diseases like chronic venous insufficiency, Varithena may not be the best treatment.
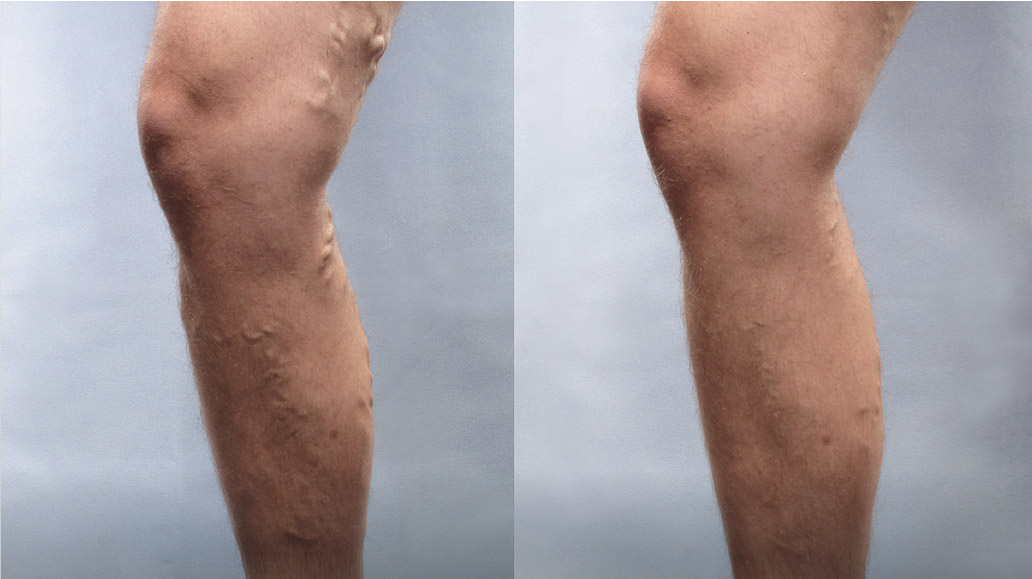
Before & After
Frequently Asked Questions
Chronic venous insufficiency is a type of vein disease in which veins have increased pressure and are unable to allow blood to flow back up from your legs to your heart. Veins have valves that prevent blood from flowing in the wrong direction. However, when these valves don’t work well, the blood flows backwards, causing the blood to pool in your legs. If you have chronic venous insufficiency, you might have varicose veins, edema or leg swelling or even venous leg ulcers.1
Varicose veins and vein disease are enlarged, often bluish, twisting leg veins that bulge above the surface of the skin. It is a common condition affecting many men and women. They can cause uncomfortable symptoms such as heaviness, achiness, swelling, throbbing and itching (HASTI™).
Spider veins are smaller and look more like branching veins and can be found on the legs or face. Typically, spider veins are not accompanied by the HASTI symptoms. Your doctor can determine if spider veins have underlying vein issues that could lead to varicose veins.
Varicose veins occur when one-way valves that regulate the direction of blood flow become weakened and no longer function properly. Instead of blood moving toward the heart, weakened vein valves can cause blood to leak back into the veins causing them to enlarge.
Varicose veins can and often do get worse if left untreated. In the Edinburgh Vein Study, chronic venous disease progressed in more than 57% of the patients with varicose veins or chronic venous insufficiency over 13 years of follow-up.2
Common risk factors include family history, aging, gender, pregnancy, being overweight, lack of movement, history of deep vein thrombosis and working at jobs requiring prolonged standing.
Venous leg ulcers are a symptom of advanced chronic venous insufficiency. Certain factors put you at increased risk for venous leg ulcers, including varicose veins, obesity, standing for long periods of time (usually for work) and having a history of blood clots in your legs. 1 in 4 Americans 65 and over will have a venous leg ulcer in their lifetime.3
Venous leg ulcers are caused by high pressure in the lower leg veins, called venous hypertension. When this pressure continues, it damages the skin, which breaks down and forms an ulcer. Symptoms of venous leg ulcers Venous leg ulcers can be unsightly and painful wounds that develop around your ankle. They typically look like large, shallow wounds with uneven edges. Other symptoms4 can include achiness, swelling, throbbing, itching and skin changes.
References
1 National Institutes of Health. Venous Insufficiency. MedlinePlus website. https://medlineplus.gov/ency/article/000203.htm. Accessed February 2023.
2 Lee et al. J Vasc Surg Venous Lymphat Disord. 2015;3(1):18–26.
3 Margolis et al. J Am Acad Dermatol. 2002;46(3):381-386.
4 https://health.clevelandclinic.org/leg-sores-wont-heal-whatscausing-your-venous-leg-ulcers/
